The world of mental health care increasingly relies on a structured and documented approach to patient care. One such approach is the Soap Notes Counseling Template, a system designed to capture detailed information about a client’s session, facilitating continuity of care and providing valuable insights for therapists. This template isn’t just a collection of notes; it’s a tool for building a comprehensive understanding of the client’s experience and needs. Soap Notes Counseling Template is becoming a standard practice in many therapeutic settings, offering a significant advantage in terms of patient outcomes and therapist efficiency. It’s a shift towards a more holistic and client-centered approach to therapy. Understanding the principles behind this template and its benefits is crucial for anyone involved in providing mental health services. This article will delve into the structure, purpose, and practical applications of the Soap Notes Counseling Template, equipping you with the knowledge to effectively utilize it.
Understanding the Core Principles
At its heart, the Soap Notes Counseling Template is built on the principle of detailed documentation. It moves beyond simply recording what the client says to capturing the how and why behind their experiences. This includes observations about the client’s body language, emotional tone, and the specific details of the session – everything that informs the therapist’s understanding. The template emphasizes capturing not just the content of the session, but also the context within which it occurred. This contextual awareness is vital for accurate diagnosis and effective treatment planning. Furthermore, the template encourages a consistent and organized approach to note-taking, promoting clarity and reducing the risk of miscommunication. It’s about creating a shared understanding between therapist and client, fostering trust and collaboration. The template’s success hinges on its ability to be easily accessible and readily usable by the therapist, minimizing the burden of note-taking and maximizing the value of each session.
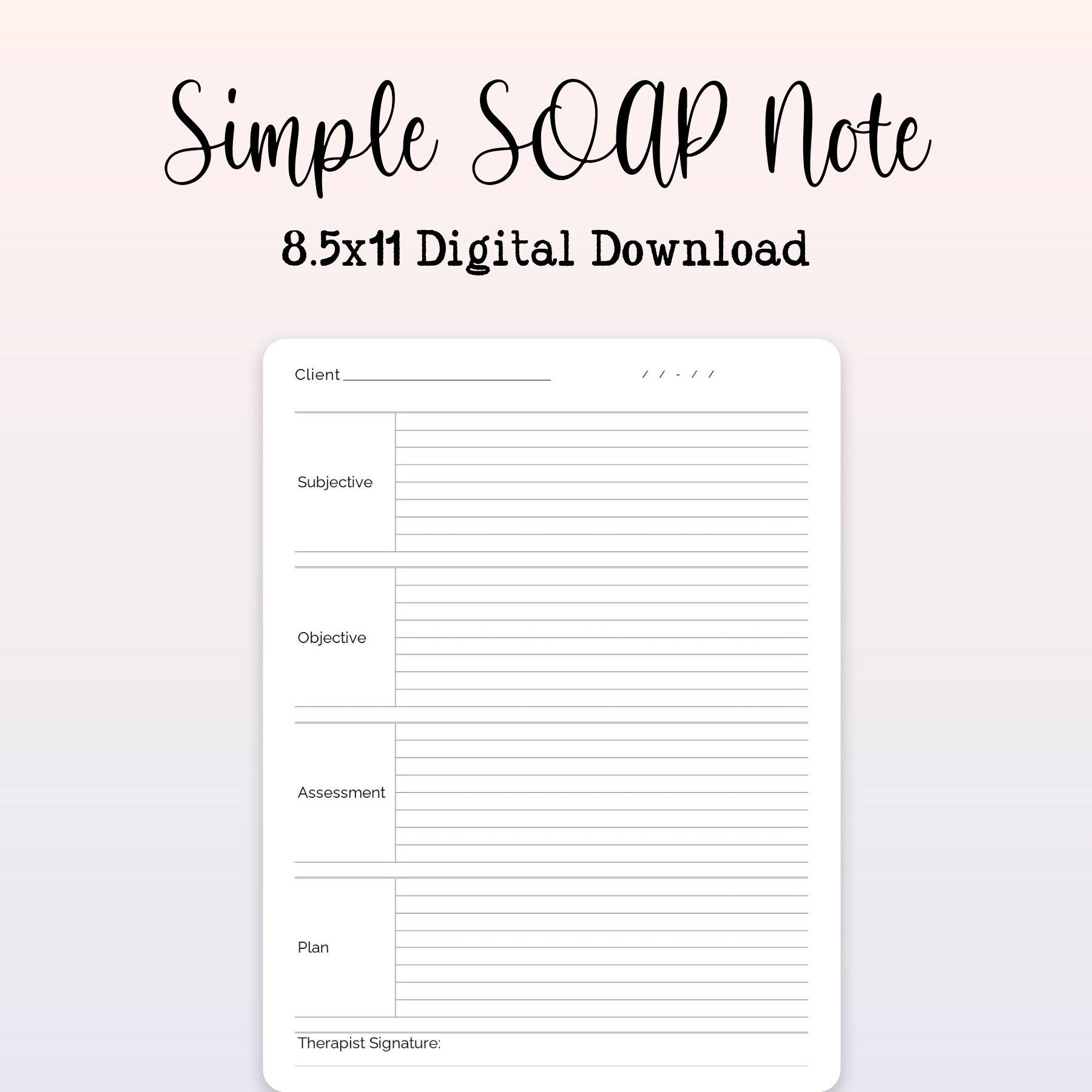
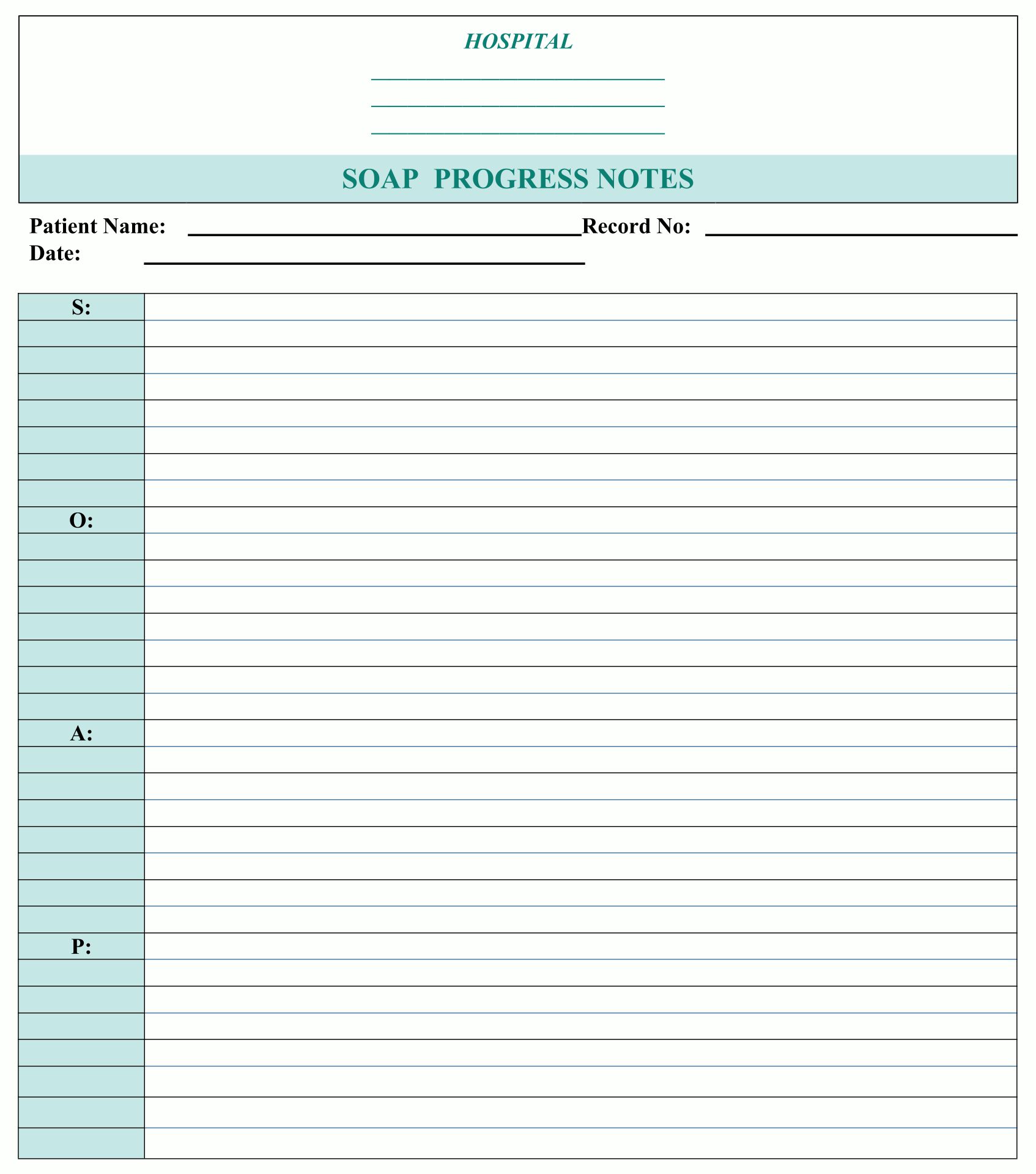
The Template Structure: A Step-by-Step Guide
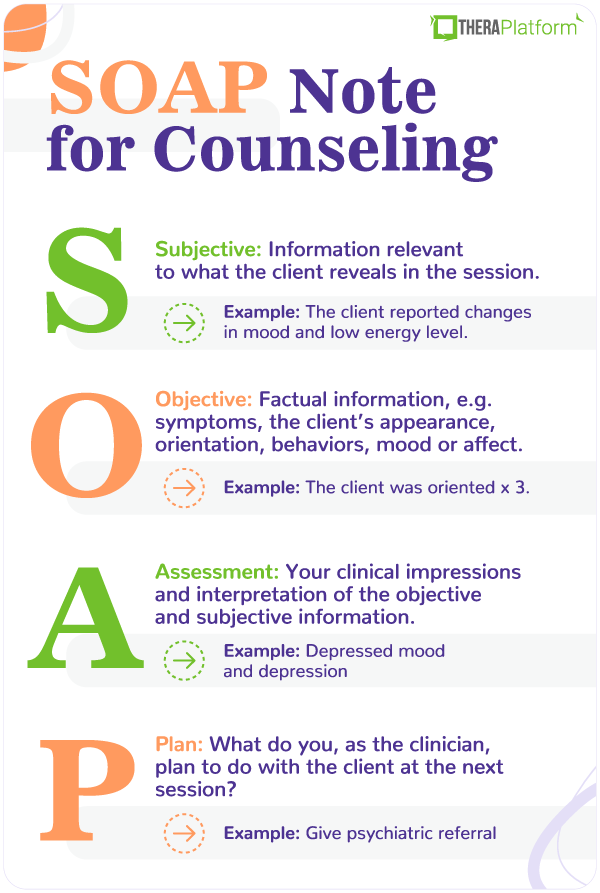
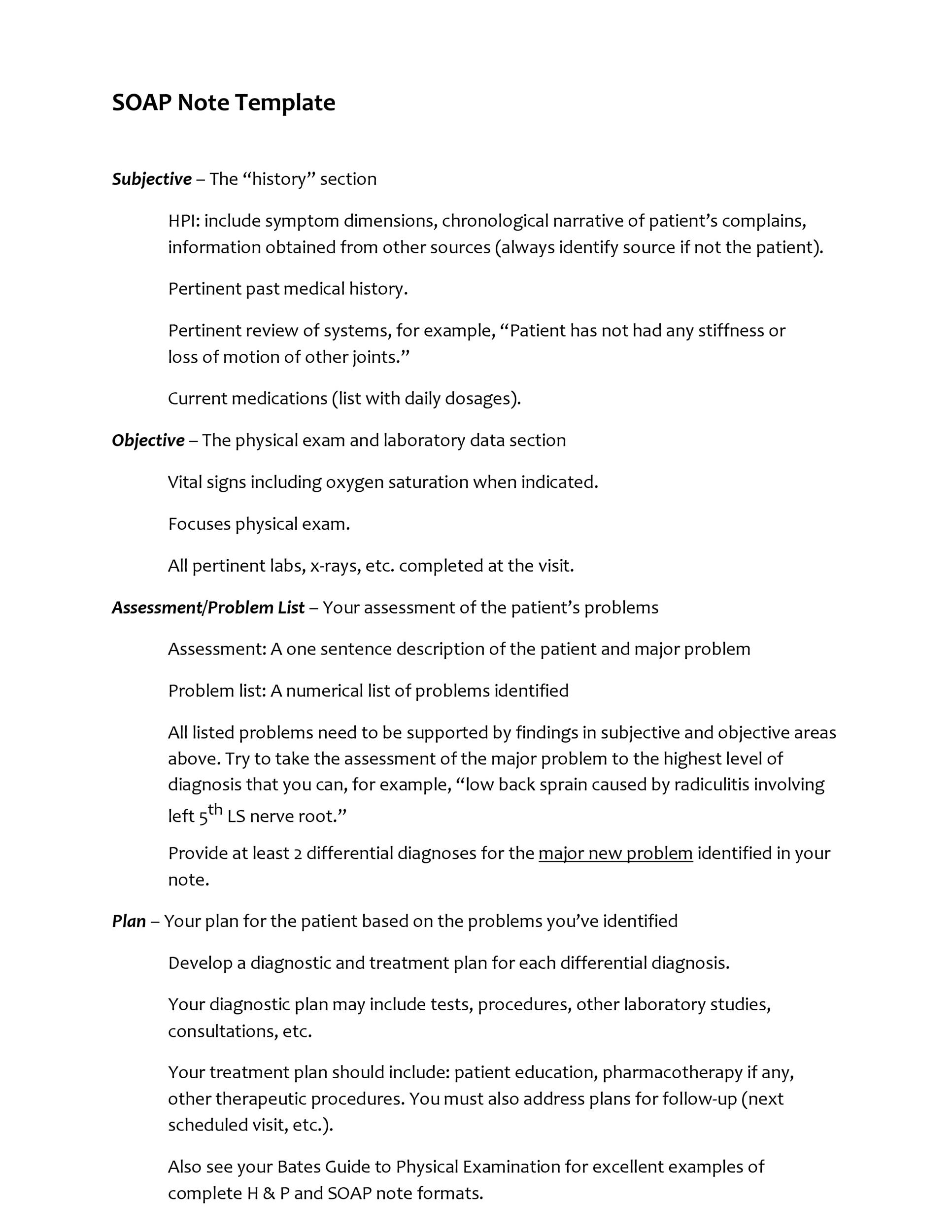
The Soap Notes Counseling Template is typically structured in a way that allows for easy retrieval and analysis. It generally includes the following sections:
- Client Information: This section gathers basic demographic data, including client’s name, date of birth, contact information, and any relevant clinical history.
- Session Summary: A brief overview of the session’s purpose, goals, and any relevant interventions.
- Client’s Presentation: This section details the client’s current state, including any reported symptoms, concerns, and emotional experiences. It’s crucial to capture the client’s perspective – what they are feeling and experiencing.
- Therapist’s Observations: This is the core of the template, where detailed notes are recorded about the session’s dynamics, the client’s behavior, and any relevant observations. This section requires careful and objective writing.
- Therapeutic Interventions: A record of the interventions used during the session, including the rationale behind them and the client’s response.
- Plan of Action: A clear and specific plan outlining the next steps for the client, based on the session’s content and the therapist’s assessment.
- Signature and Date: A formal signature and date to confirm the session’s documentation.
Section Breakdown: Key Areas of Focus
Let’s examine some of the key areas that should be thoroughly documented within the template:

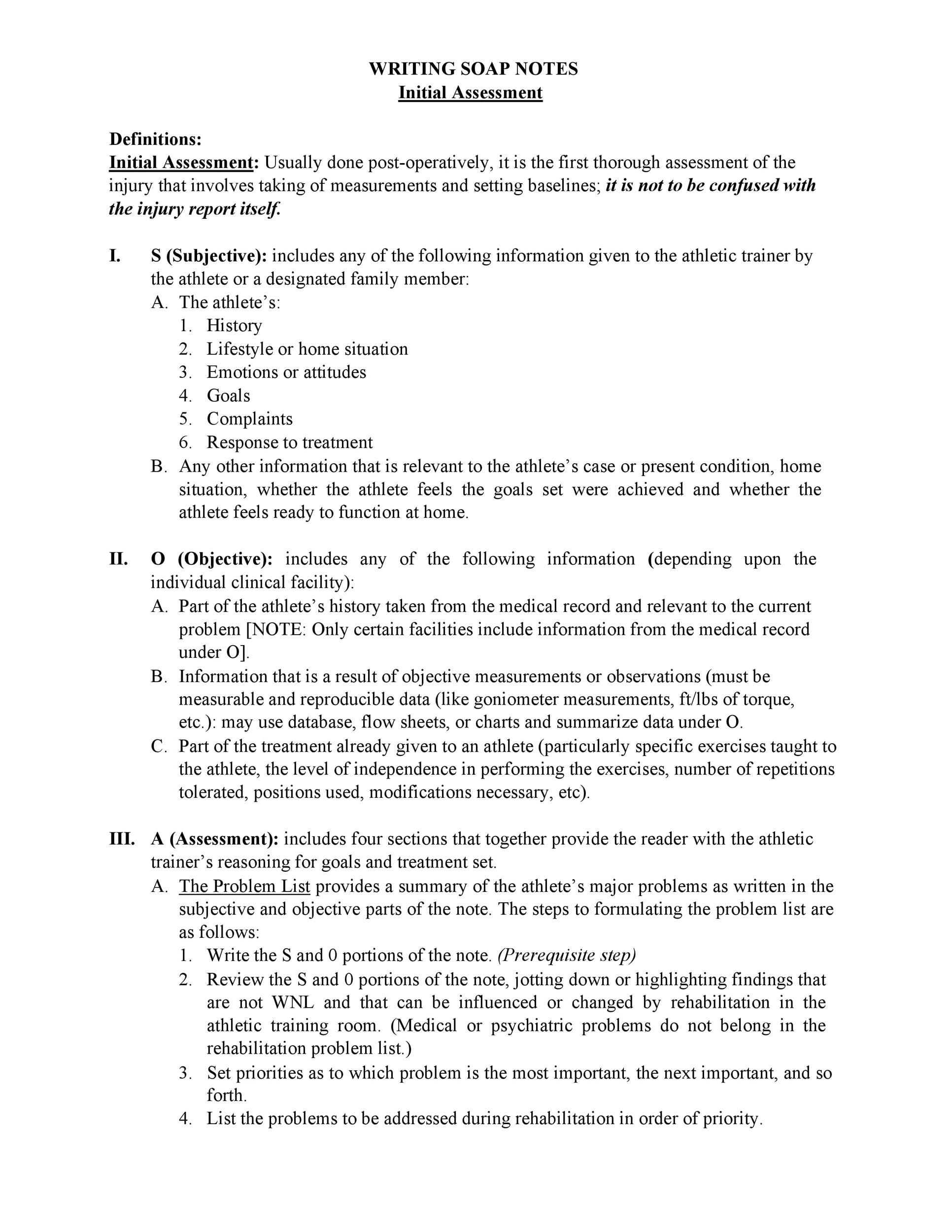
1. Client’s Presentation – Understanding the “Why”
This section is paramount for accurately portraying the client’s experience. It’s not enough to simply state what the client said; the therapist must capture the emotional context behind their words. For example, instead of simply noting “Client reported feeling anxious,” the therapist should document “Client expressed feelings of anxiety regarding upcoming presentation, citing fear of judgment and potential negative feedback.” This detailed observation allows for a deeper understanding of the underlying issues driving the client’s behavior. This section is vital for identifying patterns and potential triggers.
2. Therapeutic Interventions – What Worked and What Didn’t
The therapist’s role is to meticulously record the interventions employed during the session. This includes the specific techniques used (e.g., Cognitive Behavioral Therapy, mindfulness exercises), the rationale behind their application, and the client’s response to each intervention. It’s important to note whether the intervention was effective and, if not, why. For instance, “Client demonstrated increased relaxation through deep breathing exercises, which appeared to reduce anxiety levels.” This level of detail allows for informed adjustments to treatment plans.
3. Observations – Beyond the Words
This section goes beyond simply recording what the client said. It’s about observing how the client presents themselves – their body language, facial expressions, tone of voice, and overall demeanor. For example, “Client appeared withdrawn and hesitant during the discussion of their past relationship difficulties, exhibiting signs of avoidance.” These observations provide valuable insights into the client’s emotional state and can be crucial for identifying potential barriers to progress. Pay close attention to non-verbal cues.
4. Detailed Notes on Therapeutic Dynamics
This is where the template truly shines. It encourages the therapist to document the interaction between the client and therapist – the dynamics of the session, the flow of conversation, and any moments of connection or disconnection. This includes noting any shifts in the client’s engagement, the therapist’s responsiveness, and any challenges encountered during the session. For example, “Client expressed a sense of vulnerability during the discussion of their childhood trauma, demonstrating a willingness to share personal experiences.”
5. Plan of Action – Moving Forward
The Plan of Action section is crucial for ensuring continuity of care. It should clearly outline the next steps for the client, based on the session’s content and the therapist’s assessment. This might include scheduling a follow-up appointment, providing homework assignments, or referring the client to other resources. The plan should be specific, measurable, achievable, relevant, and time-bound (SMART). A well-defined plan is essential for preventing setbacks.
The Importance of Consistency and Accuracy
The effectiveness of the Soap Notes Counseling Template hinges on its consistency and accuracy. Therapists should adhere to a standardized format and ensure that all notes are thoroughly and objectively documented. Regular review and revision of the template are also recommended to ensure it remains relevant and effective. It’s a tool that requires ongoing refinement and adaptation to meet the evolving needs of the therapeutic process. Furthermore, training and support for therapists in utilizing the template effectively are crucial for maximizing its benefits.
Benefits of Utilizing the Soap Notes Counseling Template
The adoption of the Soap Notes Counseling Template offers a multitude of benefits for therapists and clients alike. For therapists, it streamlines the documentation process, reduces administrative burden, and enhances the quality of patient care. For clients, it provides a clear and comprehensive record of their therapeutic journey, fostering greater understanding and facilitating effective communication with their therapist. The template’s structured approach promotes accountability and facilitates data-driven decision-making. Ultimately, it contributes to a more collaborative and patient-centered therapeutic environment.
Conclusion
The Soap Notes Counseling Template represents a significant advancement in the practice of mental health therapy. Its structured approach, emphasis on detailed documentation, and focus on client-centered care make it a valuable tool for therapists seeking to improve patient outcomes and enhance the therapeutic process. By consistently utilizing this template and adhering to its principles, therapists can unlock its full potential and provide truly effective and personalized care. The continued evolution of this template, incorporating technology and best practices, will undoubtedly shape the future of mental health therapy. Soap Notes Counseling Template is more than just a document; it’s a commitment to a deeper, more meaningful connection with the client.